Researchers from Tel Aviv University and Sheba Hospital believe that the new discovery may contribute to the development of a vaccine against melanoma.
By Pesach Benson, TPS
A discovery of the way melanoma spreads has a group of Israeli researchers confident that their findings will contribute to the development of a vaccine against the deadly form of skin cancer.
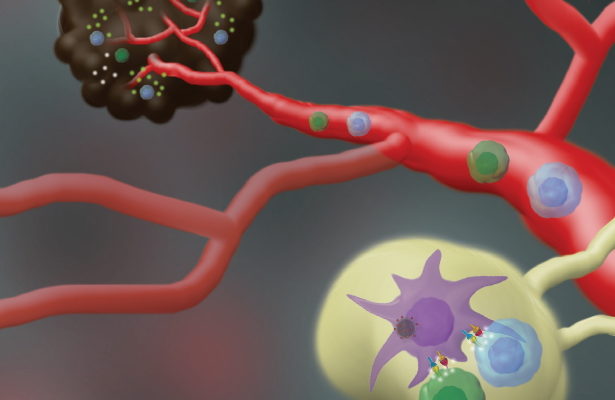
The study by a team of researchers from Tel Aviv University and the Sheba Medical Center in Ramat Gan found that melanoma cancer cells spread by manipulating their surrounding environment — specifically by creating new lymph vessels in the top layers of skin collectively known as the dermis.
Melanoma and other forms of skin cancer are typically caused by too much exposure to ultraviolet rays from the sun, tanning beds or sun lamps. Risk factors include light natural skin color, skin that freckles or burns easily in the sun, and a family history of skin cancer. Once melanoma forms, it can spread to other parts of the body normally covered.
According to the World Health Organization, 325 000 new cases of melanoma were diagnosed worldwide and 57 000 people died from the disease in 2020.
Melanoma starts with uncontrolled division of melanocyte cells in the epidermis – the top layer of the skin. In the second stage the cancer cells penetrate the dermis and metastasize through the lymphatic and blood systems. In previous studies a dramatic rise was observed in the density of lymph vessels in the skin around the melanoma – a mechanism that was not understood by researchers until now.
The research team was led by Prof. Carmit Levy of Tel Aviv University and Prof. Shoshana Greenberger of the Sheba Medical Center. Their findings were recently published in the peer-reviewed Journal of Investigative Dermatology.
Since melanoma is not dangerous at the premetastatic stage — before the cells spread to other parts of the body — understanding the mechanism by which the metastases spread via the lymphatic and blood systems can hopefully contribute to the development of a vaccine against this deadly cancer, the researchers said.
“Melanoma confined to the skin is not life-threatening,” Greenberger said. “Hence, the most promising approach to combat melanoma lies in immunotherapy. We aim to develop a vaccine that stimulates the immune system to target melanosomes, specifically attacking the lymphatic endothelial cells invaded by these vesicles. By halting the mechanisms that generate metastases in lymph nodes, we can effectively impede the disease’s progression.”
She said, “We demonstrated for the first time that in the first stage, in the epidermis, melanoma cells secrete extracellular vesiculas called melanosomes. What are these vesiculas and how do they impact their environment? Examining this in human melanomas from the Pathology Institute, we demonstrated that melanosomes can penetrate lymph vessels.”
Greenberger added, “Then we examined their behavior in the environment of actual lymph vessel cells and found that here too the melanosomes penetrate the cells and give them a signal to replicate and migrate. In other words, the primary melanoma secretes extracellular vesiculas that penetrate lymph vessels and encourage the formation of more lymph vessels near the tumor, enabling the melanoma to advance to the lethal stage of metastasis.”
To lower the risk of skin cancer, experts recommend staying in the shade, wearing clothing that covers the arms and legs, and wearing a wide-brimmed hat to protect the face, head and neck.
Wraparound sunglasses that protect from UVA and UVB rays and sunscreen with a sun protection factor (SPF) of 15 or higher are also advised.